The United States is the greatest country in the world. Or is it?
It would seem pragmatic to consider one of the wealthiest countries in the world to have an effective healthcare system; however, the U.S. has been long criticized for its failure to provide citizens with universal healthcare.
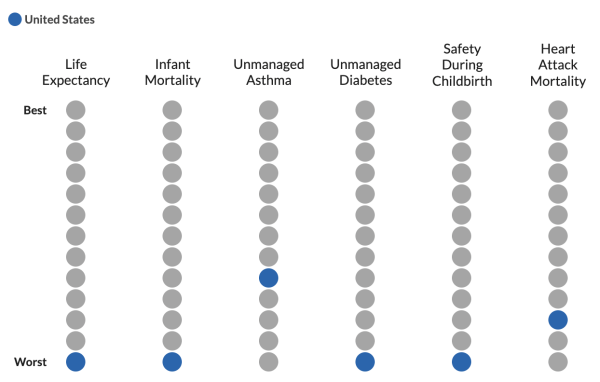
According to the Peter G. Peterson Foundation, the U.S. also performs the worst in many basic health standards in comparison to countries of similar wealth. Some areas of poor performance include infant mortality, life expectancy, safety during childbirth, and unmanaged diabetes in the U.S.
American standards have long reflected our emphasis on the importance of efficiency; yet, our healthcare system contradicts it.
By engaging in the tedious process of formally scheduling an appointment with a doctor for the most minor illness, American citizens lose the opportunity to do more productive activities.
Melanie Riker, a working mom in the town of Wilton, Connecticut, voices her concerns: “The process is very time-consuming. Because often I will call, they may not be open, and sometimes they are closed for lunch between 12 and 1,” she says. “And so you’re leaving a voice message and they call you back and then if you’re working you’ll never get them back on the phone. Finally, I may connect with somebody and we’ll make an appointment. A sick visit could typically happen that day. For a good visit, it’s usually months out before I get to see the doctor.”
For working parents, this system presents significant inconveniences and challenges. According to Sidecar Health, the average doctor’s appointment fee without insurance ranges from $99 – $152 in Connecticut. Having to take time off from work to bring a child to the doctor for a minor cold – something that may still require a medical evaluation – causes even more economic stress on families.
Despite these troubles, some individuals believe that their healthcare problems have been solved with the Affordable Healthcare Act (ACA). In 2010, 16% of Americans were uninsured; by 2016, the uninsured rate dropped to 9%. The Center for American Progress (CAP 20) states that nearly 20 million Americans have gained health insurance coverage since the enactment of the ACA.
Although beneficial, the ACA does not eliminate healthcare costs by any means, as 30 million Americans are still uninsured. It also does not dissolve the problem of accessibility. In a study conducted by the American Academy of Physician Associates, 65% of adults believe that the healthcare system feels “overwhelming” and “time-consuming.” This high number jumps to 76% for young adults aged 18 to 34. The study also found that individuals who cannot get an appointment in the same week wait roughly a month to see a doctor for needed appointments. The same survey also found that 44% of adults skipped or delayed visits in the past two years, 40% of whom were concerned about the cost, and 30% could not take time away from their responsibilities.
Dr. Tochi Iroku-Malize, the president of the American Academy of Family Physicians and the chair of family medicine for Northwell Health in New York sees similar patterns. With families having to choose between going to the doctor or paying for rent and food, “the health issue is no longer the priority,” she told The New York Times.
Our healthcare system is failing us. For a country to thrive, basic access to healthcare proves to be indispensable.
In contrast to its American counterpart, European healthcare depends on pharmacies smoothly integrated into society, with pharmacists playing a more active role in the medical field. Rather than simply providing over-the-counter medications and prescriptions like CVS or Walgreens, these pharmacies often provide personalized consultations, thorough medical advice, and minor medical treatments while also being able to provide prescriptions and over-the-counter drugs in a more productive manner.
Grant Vogelman, a sophomore at Wilton High School who lived in Geneva, Switzerland for a year, says that to get a prescription from your local pharmacy “took about five minutes.” The efficiency of such a system arises from the fact that “you’re not going to wait in line for a really long time” due to the widespread presence of pharmacies. He also adds that the pharmacies are “a lot cleaner, well stocked, well organized, and accessible.”
In contrast to the smooth process of getting a prescription in Switzerland, Riker says, “You have to see the physician first before they can write a script, and then they send it in and sometimes it takes quite a bit of time before it gets to the pharmacy – let’s say CVS – for it to be filled. Or sometimes they’ll send it to the wrong pharmacy and then there are wires crossed. It’s a very frustrating process.”
Roberta Niculescu, an avid traveler, experienced the efficient process of European pharmacies in her recent trip to Portugal. “I had developed a cold sore at the beginning of our trip. I went to a pharmacy and put on the cream they gave me – it vanished within a day and only cost me $5.… Usually in the U.S., any cream you can get over-the-counter is not as effective and often more expensive.”
“When I came back to the States, my doctor informed me that the same cream was only reachable by prescription,” Niculescu added. “This is such an inconvenience for something as simple and common as a cold sore.”
Niculescu’s account demonstrates the stark comparison in both efficiency and financial means between European and American healthcare.
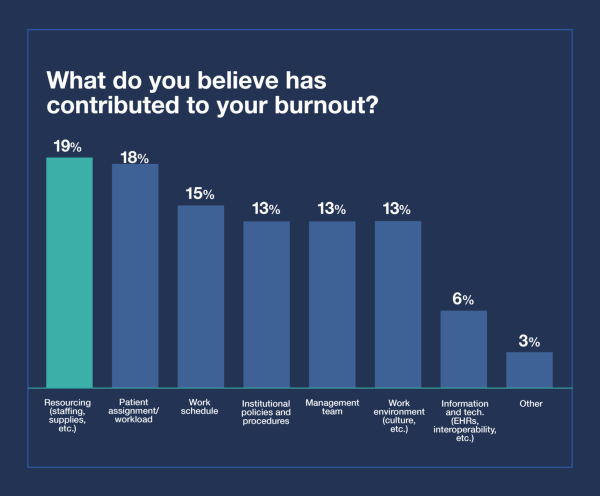
In addition to arguments for accessibility and cost reduction, pharmacies would also aid doctors and hospital staff. Since April of 2022, about “266,900 healthcare workers reported working overtime – the highest number ever,” according to The National Library of Medicine. Another survey from the organization showed that as of 2022, 45% of 4,467 practicing nurses reported severe burnout, and over half of early and mid-career nurses said they considered leaving their jobs in the following year.
Using pharmacies as an efficient location where clients can get diagnosed, fill prescriptions, and pick up those prescriptions all in one sitting would lower the demand for nurses and doctors significantly; this can be done by targeting patients with minor illnesses whose support only requires simple medications.
Vogelman recalls that they would go to the pharmacy “if you have a fever, or if there was a cold going around we would go to the pharmacy then. It was really whenever you were sick.”
Riker brought her kids to the doctor for similar reasons: “My kids needed attention for colds, bronchitis, strep, ear infections, pink eye, flu, and allergies.”
Furthermore, easing doctor’s schedules would allow them to focus on more serious patients and provide higher-quality research and performance that they are not able to do today. This in turn could put the United States at a higher ranking for healthcare and boost the country’s economy.
Poor health acts as the biggest restraint in activities and experiences. Future generations must prioritize health if they wish to consider the United States the “greatest country in the world.”
Only with the development of pharmacies that have the capability of diagnosing and prescribing medications can the United States aid its citizens in both financial and productive means, prevent burnout among healthcare workers, and regain prestige when considering U.S. healthcare.


